Helping your child live a healthy life with asthma
The hongi symbolises the breath of life.
It recalls the moment when Tāne breathed life into Hineahuone, the first earthly woman.
Introduction
Asthma is a common New Zealand illness, but it’s scary when it affects the child you care for. The good news is that asthma can be well managed.
This booklet is for the parents, whānau, and other caregivers of children with asthma. It will help you make sure your child stays fit, healthy, and happy. You will learn how to help prevent an asthma attack and what to do when one takes place.
There’s also a digital resource online at:
It includes video clips and animations that you and your child could view together.
You don’t need to read the booklet all at once. You can just dip in and out of it. It will help you to answer these questions:
- What is asthma?
- What are the symptoms of asthma?
- What are the triggers for asthma?
- How is asthma treated?
- What should I do to manage my child’s asthma?
- What should I do in an emergency?
- Should my child be physically active?
- Who can help?
- Who are our asthma health providers?
What is asthma?
Asthma is a common illness of the respiratory system. In New Zealand, one child in seven needs to take medicine for asthma.
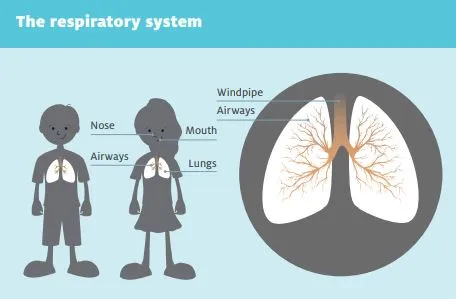
The respiratory system is the system through which we breathe. We breathe in to bring oxygen into our bodies, and we breathe out to remove carbon dioxide. The respiratory system includes the nose, mouth, lungs, and a set of airways.
The largest airway is the windpipe, which connects the lungs to the nose and mouth. There are more airways inside the lungs. The airways are also called breathing tubes.
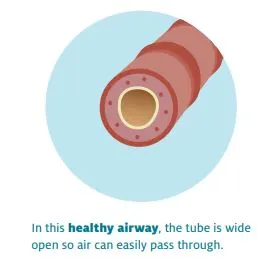
People with asthma have sensitive airways. Your child’s sensitive airways may be irritated by a trigger in the environment (such as pollen), by an illness, or by an emotion (such as anxiety). The irritation makes your child’s airways swell up so that it becomes difficult to breathe. You can read more about asthma triggers further below.
What happens in an asthma attack?
Most people can keep their asthma under control for most of the time. You can teach your child to notice the signs of asthma and what to do to stop having a full asthma attack or ‘flare-up’.
Knowledge is power and you can use this power to help prevent your child having an asthma attack. You need to know your child’s body, know what triggers your child’s asthma, and make sure your child always takes their medicine.
Renee’s son Alex has a severe form of asthma that’s complicated by a restriction of the throat, but he’s also a keen sportsman.
Alex’s asthma is serious, but it’s never stopped him pursuing his passion for sport! There’s been running, football, and underwater hockey, and these days he’s into rowing.
I’ve been so impressed with how Alex has taken it all in his stride. Even when he was quite young, he’s wanted to work with us all to find out how to stop getting sick and get things right again when he is. These days, he confidently discusses his action plan with his doctor and practice nurse and takes on a lot of the responsibility for carrying them out.
What are the symptoms of asthma?
It’s important to know the symptoms of asthma. Asthma can usually be quickly managed, but it is dangerous if it is just left.
Asthma has four main symptoms:
- coughing
- breathlessness
- wheezing
- a tight feeling in the chest.
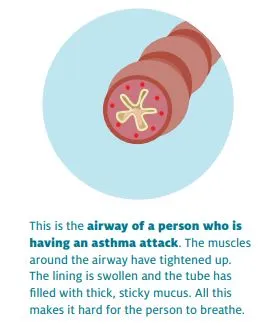
Wheezing is a whistling sound that people make when they are trying to breathe through airways that are narrower than usual. It is often louder when trying to breathe out.
In an asthma attack, these symptoms get worse, so the person finds it difficult to breathe. Some people say it feels like they have something heavy on their chest or it feels tight. It can be so hard to breathe that it becomes painful.
What does it feel like?
To get an idea of how asthma feels for your child, try breathing in and out through a straw. First do it normally. Then pinch the straw’s end and keep trying to breathe in and out. You will start to feel short of breath and you may feel tightness in your chest.
If you don’t have a straw, try blowing air through an open fist. Then gradually close your fist, still trying to blow through it. Imagine how tiring this would feel!
Very young children can’t tell people how they’re feeling. They need other people to keep an eye out and notice when symptoms start to appear.
You might notice that your child is getting tired because their difficulty in breathing makes it hard to sleep. In a more severe case, you might see your child’s chest and sides pulling in.
With an older child, you can ask how they’re feeling and help them to watch out for asthma symptoms for themselves.
Your doctor may give you a symptom diary. You and the doctor can use this diary to keep track of what is happening and understand the patterns in your child’s symptoms. You can read more about symptom diaries further below.
What are the triggers for asthma?
In the past, some people thought that asthma was ‘all in the head’. Now we know that it is the body’s response to a trigger that causes someone’s airways to become narrow.
The triggers can be different for different people, but there are some that are very common.
In the left-hand side of the table below, you can see some common triggers for asthma.
In the right-hand column, there are some suggestions for how you can help your child avoid these triggers.
Talk to other people who know your child well about possible triggers they’ve noticed.
Some of the asthma triggers, like pollen and pet fur, contain allergens. Allergens are tiny substances that are usually harmless, but they can cause an allergic reaction in some people.
| Common asthma triggers | Some ways to help your child avoid asthma triggers |
| Colds and flu |
All children get colds. When this happens, watch carefully for signs of asthma. Be ready to change your child’s medicine in line with their action plan. Make sure your child is immunised in autumn each year. The flu vaccination is free to all children who are on preventative asthma medication. |
| Cigarette smoke | Keep your child’s environment auahi kore (smokefree). There’s lots of help if you want to give up smoking. Start with your doctor or nurse or try Quitline. |
| Cold dry air or changes in the weather | Keep your child warm and dry and use a scarf to cover their mouth and nose. Encourage your child to warm the air by breathing in through their nose instead of their mouth. If their nose is usually blocked, discuss this with your doctor. |
| Stress and anxiety | Do what you’re already doing to keep your child strong and healthy through proper rest, good food, exercise, and taking the time to talk through any worries. Relaxed breathing reduces stress and anxiety. |
| Mould | Try to keep your house warm, dry, and well aired. Vent your laundry dryer to the outside and use extractor fans in the kitchen and bathroom. If possible, use a dehumidifier. Treat any mould with diluted household bleach, but be careful not to breathe in the fumes. |
| The pollen in some plants | Pollen is a common trigger, especially in summer and in the early morning and evening. Try to keep outdoor activities for the early afternoon. Close windows when it is windy or humid. Choose pretty, brightly coloured plants for the garden that use insects to transfer their pollen, instead of the wind. |
| Cats and other furry pets |
Don’t get a pet without first checking whether your child is allergic to it. If you can’t avoid having a furry pet, talk to your vet about how to keep it well groomed. If you go to a house where there is a furry pet, ask for the pet to be put outside. Your child should never sleep in a room with a pet. If you move into a house that has had a pet, you will need to clean it thoroughly. It can take three to four months of regular deep cleaning to get rid of all the allergens. |
| Dust mites |
All houses have some dust mites, but there are ways you can keep them down. For example, you can:
|
| Physical activity | Exercise is good for everybody, including people with asthma! However, it can trigger asthma, especially when the air is cold and dry. On page 25 there is information about how your child can exercise safely and happily |
| Food | Very few children are allergic to food like cow’s milk, wheat, seafood, eggs, soy, and peanuts. If you think a food is triggering your child’s asthma, visit your health provider (for examples of health providers, see below). There are simple tests the health provider can run to check whether food is the problem. If it is, your health provider can suggest other healthy foods to replace it. |
You know your child better than anyone. You can use your knowledge to help your child avoid the triggers for their asthma. Your child won’t always be able to avoid their triggers, but by knowing what they are, you can help manage them.
Most kids will be exposed to triggers like exercise, animals, and grass, and sometimes that will mean their asthma plays up. I don’t think that parents need to feel guilty that their child with asthma is living a normal life.
Tāne, asthma expert
How is asthma treated?
Asthma cannot be cured, but it can be treated. In this part of the booklet, you will read about asthma medicine and the way it is delivered.
Introducing inhalers
What is an inhaler?
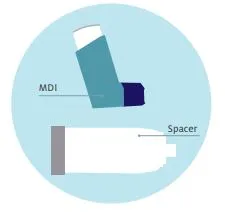
An asthma inhaler is a plastic case that holds asthma medicine. It is designed to deliver the medicine directly to the lungs. Inhalers are often called puffers. There are two types of inhaler: metered dose inhalers (MDIs) and dry powder inhalers.
Metered dose inhaler
A metered dose inhaler (MDI) delivers a set amount of asthma medicine. The MDI contains a pressurised canister that holds the medicine in the form of gas. The MDI needs to be shaken to mix the medicine before it is used. When the MDI is pressed, the canister releases its gas into a spacer.
A spacer is a clear plastic tube. The inhaler fits in one end of the spacer and the other end of the spacer has a mouthpiece, or a mask which fits into the mouthpiece. A valve in the mouthpiece of the spacer opens and shuts as the person using it breathes in and out. The medicine goes directly into their lungs so that it can start working straight away.
Spacers greatly increase the effectiveness of the asthma medicine. You can get a spacer free of charge from your health provider.
What if my child is very young or doesn’t like the inhaler?
Children under the age of four can use their MDIs with a mask attached to the spacer. You or another adult will need to help them.
Once the spacer is in your child’s mouth or the mask is over their mouth and nose, squirt the medicine into the spacer. It will remain suspended there, giving your child time to take six normal breaths through the mask.
The mask can come off the spacer when your child is able to use the spacer mouthpiece. For most children, this is by the age of four.
Dry powder inhaler
The medicine in a dry powder inhaler is not a gas but a powder. This inhaler does not need to be shaken before you use it. The child breathes in the medicine directly from the inhaler’s mouthpiece. Ask your doctor, nurse or pharmacist to show you how to use the inhaler.
Using an inhaler with a spacer
The photographs below sets out six steps for using an MDI with a spacer. Younger children will need your help to follow these steps. As your child gets older, they will be able to do it themselves.
|
If using a mask, fit it to the spacer. |
Hold the inhaler upright and give it a good shake.
|
Fit the inhaler into the opening at the end of the spacer. |
|
Seal lips firmly around the mouthpiece or place the mask so it seals around the nose and mouth. |
Press the inhaler once only. |
Hold the spacer in place while taking six slow breaths through the mouth. |
If your child needs another dose, repeat steps 2 to 6.
The medicine can only help your child if it gets into their lungs. It takes time to learn to use an inhaler, and people can forget. If you’re not sure your child is using their inhaler correctly, ask your health provider to show you again.
How do I care for my child’s spacer and inhaler?
Wash the spacer once a week. This stops the medicine sticking to the side or blocking the valve. You should wash it in warm water with a mild detergent and then let it air dry.
Your child needs a new spacer every year. You can get this at the same time as you see your health provider about your child’s action plan.
MDIs should also be washed weekly. You can use this time to check that there is still plenty of medicine left and that it hasn’t reached the expiry date.
Washing your MDI
- Remove the plastic mouthpiece cap.
- Remove the metal canister but don’t put it in the water.
- Rinse the mouthpiece and cap under warm water for at least 30 seconds.
- Shake off any excess water and allow to air dry thoroughly.
- Put the metal canister back in and replace the cap.
Introducing medicines
What are the medicines for asthma?
There are several types of asthma medicine: preventer medicines, reliever medicines, combination medicines, and oral steroids. It’s important to know the differences between these medicines, to take them correctly, and to be aware of the possible side effects. The tables below will help you with this.
An ‘oral steroid’ is an asthma steroid medicine that is swallowed. It comes as a pill or a liquid.
Some children with asthma will be on a preventer medicine. Remember that asthma cannot be cured. This means it is important that your child keeps taking their preventer medicine as prescribed by your doctor.
Preventer medicines contain steroids. Steroid medicines can have side effects, but these are mild and not nearly as bad as the effects of uncontrolled asthma. Talk to your health provider – your doctor, practice nurse, or asthma educator – if you’re worried.
Even after asthma has been brought under control, it can flare up again. When that happens, you need to know which inhaler your child should use. Make sure you know the colour of your child’s preventer inhaler and the colour of their reliever. You might want to write your own label to be sure.
Most children can manage their own asthma medicine from about the age of seven. However, even much older children need you to check that their asthma is under control and help watch for any changes.
Your child may only have been prescribed one or two types of medicine, or they may have more. Your doctor will write the names of your child’s medicines on their asthma action plan. If you like, you could copy that information into the spaces in the table on the next page.
Most asthma medicine is delivered through an inhaler. For this reason, people will often talk about ‘using their reliever’ or ‘using their puffer’ rather than ‘taking their medicine’.
Preventer inhaler
| What it does |
A preventer is your child’s most important medicine. It prevents the swelling and narrowing of the airways that causes asthma. This reduces the likelihood of an asthma attack. Preventers work slowly, so your child won’t notice any immediate change in how they feel. Over time, daily use will help to keep your child’s asthma under control. |
| How to use it | Preventers need to be taken every day or as prescribed, even when your child is well. |
| Possible side effects | Possible side effects of preventer medicines include a sore throat, croaky voice, or a mouth infection. Your child can avoid these side effects by using a spacer and brushing their teeth or rinsing their mouth immediately after using their inhaler. |
Reliever inhaler
| What it does | A reliever medicine relaxes the tight bands of muscle around your child’s airways to help air flow in and out more freely. This effect should last for about two to four hours. |
| How to use it |
Reliever medicines can be taken to relieve wheezing, coughing, or tightness in the chest area. Your health provider may also suggest that your child uses it before exercise. Many people rely on their reliever inhalers to feel better immediately, but relievers do not treat the underlying cause of asthma symptoms. Uncontrolled asthma is serious and can even be life-threatening. See your health provider if your child is using their reliever inhaler more than two or three times a week because this means their asthma is not under control. |
| Possible side effects | Some side effects of reliever medicines include mild shaking, headaches, a racing heartbeat, and restlessness. If your child experiences these symptoms, see your doctor as soon as possible. |
Combination inhaler
| What it does |
Combination inhalers contain two medicines so they help prevent asthma and relieve the symptoms. |
| How to use it | Combination inhalers must be used every day, even when your child is well. Ask your health provider if this inhaler can be used in an emergency, because you may need a different reliever inhaler to use if your child is having an asthma attack. |
| Possible side effects | The unwanted side effects of a combination inhaler can include mild shaking, headaches, a racing heartbeat, a sore throat, or an infection of the mouth. Your child can avoid getting a sore throat or fungal infection by using a spacer and brushing their teeth or rinsing their mouth immediately after taking their medicine. |
Oral steroids
| What it does | Oral steroids (tablets and liquids) are very useful for bringing asthma symptoms under control when they are not settling with inhalers alone. They bring down the swelling in the lining of the child’s airways and reduce the amount of mucus produced. Only some children with asthma need oral steroids. |
| How to use it | Oral steroids are usually taken for about five days, along with your child’s preventer medicine. |
| Possible side effects |
A short course of oral steroids is safe, with no lasting side effects. Some people notice a change in mood, energy levels, or appetite. These side effects are usually mild. You can discuss the possible short-term side effects and any other concerns with your doctor or pharmacist. Very few children need long-term treatment with oral steroids. These children will be under the care of a specialist. |
What about complementary medicines?
It’s OK to try alternative approaches, such as rongoā Māori or Chinese herbal medicine, provided you discuss them with your doctor and use them alongside and not instead of prescribed inhalers and medicines. Remedies containing natural products can be dangerous for people with asthma. Remedies like bee pollen or echinacea can be a trigger for asthma, and sometimes a natural remedy can interfere with your child’s prescribed medicine.
On the other hand, traditional healing systems such as rongoā Māori are increasingly respected in mainstream medicine for taking a holistic view of health that includes the spirit, mind, body, and whānau. Some researchers are looking at the use of plant remedies, including those used by Māori, but so far there is little clear evidence about their effects. However, relaxation therapies, such as yoga, have been shown to help reduce asthma caused by stress.
If you’re thinking about trying a natural remedy, find all the information you can and talk about it with your health provider. But remember – it’s not safe to stop your child’s medicine or give them a new medicine without first having that talk.
What should I do to manage my child’s asthma?
Your doctor will have given you a child asthma action plan and you may also have been using a symptom diary. You can use the asthma action plan and symptom diary to help manage your child’s asthma and prevent an attack.
The action plan tells you what to do when your child’s asthma improves or gets worse. It tells you which medicine to use and how much. The amount and type of medicine will change with changes in your child’s asthma symptoms. The table below shows how a child’s symptoms may change from a mild asthma flare-up to an asthma emergency.
Your doctor will fill out your child’s action plan, using the information you provide. This will help you to make the right decisions. Your doctor should update it at least once a year and any time there is a change in your child’s medicine.
It is very important that you, your child, and all the people who care for your child know and understand the instructions in your child’s action plan.
The symptom diary is a place where you can record your child’s asthma symptoms so you can see any patterns over time. Seeing these patterns helps you and your health provider understand what is triggering your child’s asthma and how well the medicine is working.
You don’t need to fill in the symptom diary all the time. However, it’s very helpful when your child is first diagnosed, if there is a change in their medication, or if there seems to be a change in your child’s symptoms. As your child gets older, you can help them take responsibility for their own symptom diary.
Both the asthma action plan and the symptom diary use a traffic light system. Green means that your child is good to go… the asthma is under control. Orange means that their asthma is getting worse and your child needs to start taking their reliever medicine. Red means that this is an emergency – your child is having an asthma attack and needs help.
You can do all the right things, but your child may still have an asthma attack. Everything you are doing is helping but sometimes extra assistance is needed. In an emergency, help is at hand.
Please remember: If you have any questions, ask your doctor, nurse, or asthma educator. They’re here to help!
What should I do in an emergency?
In an emergency, try to stay calm. It helps to remember the six asthma steps: Assess, Sit, Treat, Help, Monitor, and All OK!
Assess
Assess whether the asthma attack is mild, moderate, or severe.
Mild |
Moderate |
Severe |
|
Mild symptoms indicating that asthma is worsening can include:
|
Moderate symptoms indicating that asthma is worrying can include:
|
Severe symptoms indicating an asthma emergency can include:
Dial 111 for an ambulance! |
Sit
Sit your child upright and stay with them. Lean them forward slightly and support their arms either on their knees or on a table.
Treat
Treat mild symptoms with two puffs of a reliever inhaler.
Treat moderate or severe symptoms with 6 puffs of reliever inhaler. If the reliever medicine comes in a metered dose inhaler, use a spacer. Put the spacer into the child’s mouth or use a mask for a very young child. Puff the inhaler once into the spacer and have the child breathe in and out six times. Encourage your child to breathe as normally as possible. Do this twice: one puff and six normal breaths, in and out.